What is syncope? Symptoms and Treatment options
Syncope is described as loss of consciousness due to insufficient blood flow to the brain, usually fainting or blackouts.
Vasovagal syncope is the most common type and is also known by other names such as neurocardiogenic syncope (preferred by cardiologists), vasodilator syncope, and neutral-mediated syncope. Syncope often occurs when the body overreacts to certain triggers:
Severe mental stress
- Pain
- Hungry
- Blood scene
- Standing for a long time
- Heating
- Dehydration
- Exposure to toxic odors
- Fatigue
Hyperventilation (excessive breathing leading to low levels of carbon dioxide in the blood)
The trigger causes a sudden drop in blood pressure, resulting in decreased blood flow to the brain and loss of consciousness for a time. Sometimes the heart rate drops along with the blood pressure, but often the heart rate does not change or actually increases.
Most vasovagal syncope occurs while standing, which usually occurs immediately after standing or every time the person stands up, but only occasionally, often in the case of one of the above triggers.
betist
Syncope is also a symptom of serious heart disease, such as arrhythmia, heart block, or aortic valve stenosis.
Some medications, especially antihypertensives and diuretics, are associated with an increased risk.
How common is syncope?
Syncope is a common condition. It affects 3% of men and 3.5% of women at some point in life. Syncope is more common when you are an adult, affecting 6% of people over the age of 75. This condition can occur at any age and in people with and without other medical problems.
Who gets syncope?
Syncope can occur at any age and in healthy people. Vasovagal syncope affects men and women of all ages, especially young men, especially women 12 to 25 years old.
Some people who experience syncope episodes have orthostatic hypotension. In this condition, a person’s blood pressure drops immediately or very quickly due to pooling of blood in the legs, causing blood pressure to drop rapidly. It can occur in the presence of dehydration, anemia, or over-the-counter antihypertensive medications. It is very rare due to autonomic nervous system damage or dysfunction.
Types of syncope
There are many types of syncope. The type you have depends on the cause of the problem.
Vasovagal syncope (also known as cardio-neurogenic syncope)
Vasovagal syncope is the most common type of syncope. It is caused by a sudden drop in blood pressure, which decreases blood flow to the brain. When you stand up, gravitational blood pools in the lower part of your body, just below the diaphragm. When that happens, the heart and autonomic nervous system (ANS) work to keep blood pressure stable.
Some patients with vasovagal syncope have a condition called orthostatic hypotension. This condition keeps blood vessels small (they must be) when the patient is standing. This causes blood to pool in the legs and blood pressure to drop rapidly.
Conditions synchronization
Situational syncope is a type of vasovagal syncope. It occurs only in certain conditions that affect the nervous system and lead to syncope. Some of these situations are:
- Dehydration
- Severe mental stress
- Anxiety
- Fear
- Pain
- Hungry
- Alcohol or drug use
- Hyperventilation (take in more oxygen and get rid of carbon dioxide more quickly)
- Forceful cough, dizziness, or tight neck (carotid sinus hypersensitivity)
- Syncope of micturition
- Postural syncope (also known as postural hypotension)
Postural syncope is caused by a sudden drop in blood pressure due to a rapid change in position, such as getting out of bed. Certain medications and dehydration can lead to this condition. Patients with this type of syncope typically have changes in blood pressure that drop to at least 20 mmHg (upper / systolic number) and at least 10 mmHg (lower / diastolic number) when standing.
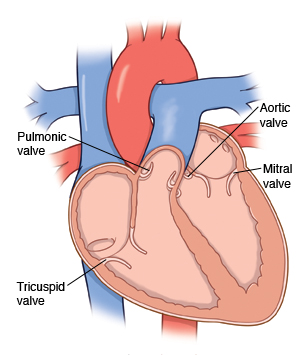
Cardiac syncope is caused by a condition of the heart or blood vessels that affects blood flow to the brain. These conditions include abnormal heart rhythm (arrhythmia), structural heart disease (blockage of blood flow in the heart), blockage of the heart’s blood vessels (myocardial ischemia), valve disease, aortic stenosis, blood clots, or heart failure. If you have cardiac syncope, it’s important to see a cardiologist for proper treatment.
Neurological syncope
Neurological syncope is caused by a neurological condition such as seizure, stroke, or transient ischemic attack (TII). Other less common conditions that cause neurological syncope are migraines and generalized hydrocephalus.
Postural orthostatic tachycardia syndrome (POTS)
Orthostatic postural tachycardia syndrome is caused by a very fast heart rate (tachycardia) that occurs when a person stands up after sitting or lying down. The heart rate is 30 beats per minute or more. The increase usually occurs within 10 minutes of standing. This condition is more common in women, but it can also occur in men.
Symptoms
Syncope episodes often precede warning signs or symptoms. These may include:
- Nausea
- Speak slow
- Weak pulse
- Changes in body temperature can make you suddenly feel boiled or cold.
- Sudden sweat from chlamydia
- Pale skin
- Obstacles to your vision, such as spots, tunnel vision, blurred vision, or seeing stretched out students
- Sounds suddenly seem too far away
- Mild headache, vaginas, or your head and body feel weightless
- Numbness
- Dizziness
- Vertigo or a feeling that moves the room.
- Rapid heartbeat
- Body weakness
- Tremor
- Headache
What Causes Syncope?
Syncope can be caused by an underlying medical condition or environmental triggers. Epilepsy can also be caused by an emotional response to a very difficult situation. Severe pain, low blood sugar, or a change in blood volume can also cause syncope. If you have low blood pressure or a heart rate, you may pass out suddenly.
Common causes of syncope:
- Low blood pressure or dilated blood vessels.
- Arrhythmia
- Sudden changes in posture, such as standing too fast, which can collect blood in the feet or legs.
- Has been standing for a long time
- Severe pain or fear
- Severe stress
- The pregnancy
- Dehydration
- Fatigue
Some people faint when they see blood. Syncope can also be triggered by multiple factors, such as if you are dehydrated or have low blood sugar. Together, even if you don’t pass out from this or the other, those two things will make you pass out.
How does syncope affect my life?
With proper diagnosis and treatment, syncope can be managed and controlled. If you have a syncope episode, you have a 30% chance of having another episode.
How your risk and condition for another episode affects you will depend on many factors, including the cause and your age, gender, and other medical problems you may have. If you have questions about your risks, talk to your doctor.
How is syncope diagnosed?
The diagnosis of vasovagal syncope often excludes other causes of epilepsy, especially heart problems.
When syncope often occurs unexplained, a doctor can use a tilt table test to see if a controlled condition can trigger an event while monitoring heart rate, blood pressure, blood oxygen level, heart rate and the symptoms. The person is placed head-up on a table that “bends” vertically at 70 degrees or more.
Blood tests can be used when appropriate to rule out other less common but serious causes, such as anemia (when your body doesn’t have enough healthy red blood cells) and adrenal insufficiency.
What are my treatment options?
Your treatment options are based on the causes of your syncope and the results of your evaluation and testing. The goal of treatment is to prevent you from having episodes of syncope.
Treatment options include:
Taking medications or making changes to medications you have already taken.
Wear support clothing or compression stockings to improve blood circulation.
Make changes to your diet. Your doctor may suggest that you eat small, frequent meals; Eat more salt (sodium); Drink more fluids, increase the amount of potassium in your diet; And avoid caffeine and alcohol.
Be very careful when standing.
Raise the head of the bed while sleeping. You can do this by using extra pillows or by placing risers under the legs at the head of the bed.
“Triggers” that prevent or change conditions or cause an episode of syncope.
Biofeedback training to monitor rapid heart rate. You can get more information by calling the Cleveland Clinic Department of Psychology at 216.444.6115 or 800.223.2273 ext, or schedule an appointment for an evaluation with a biofeedback specialist. 46115.
Treatment of structural heart disease.
Set up a pacemaker to keep your heart rate stable (only necessary for patients with certain medical conditions).
Implantable cardiac defibrillator (ICD). This device constantly monitors your heart rate and rhythm and corrects for rapid abnormal rhythms (only necessary for patients with certain medical conditions).
Your Cardiologist and other members of your health care team will develop the right treatment plan for you and discuss your treatment options with you.
If you are diagnosed with syncope, check the laws in your state. Some states require syncope drivers to contact the Licensing Office.



